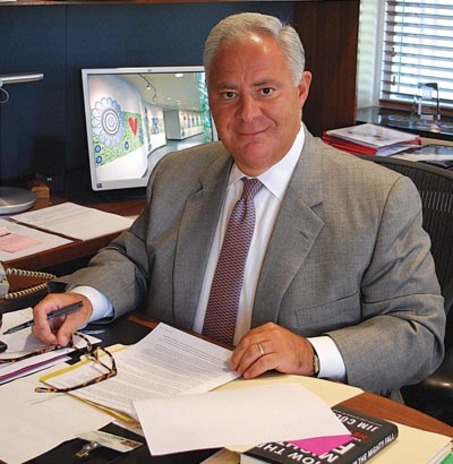
An interview with Frank Sardone, the CEO of Bronson Methodist Hospital in Kalamazoo, Michigan.
Student: What was the processes that lead to Bronson spearheading this effort of Enroll Kzoo?
Frank Sardone: Here at Bronson we have a plan for excellence. We have a vision that Bronson will be a
nation leader in healthcare quality, and we have four strategies to help us achieve this, which
we call the four Cs, they are clinical distinction, exceptional customer experiences, corporate
vitality, and community health catalyst.
So, as part of the community health catalyst initiative we had a task force, with the board
committee members being, the chair Randy Eberts, Bill Mayer and Amy Terry. They conducted
a health needs assessment for all the counties we serve, primary ones being Kzoo, Van Buren,
and Calhoun. Â We then documented what were the real needs were from a health needs stand
point and out of that, emerge a number of priorities; the priorities did differ a little between
counties, but the one that was consistent and what we wanted to focus on was, access to health
care. One of the best ways we thought to we could improve access is by getting people enrolled
in health issuance, and this is what lead to the creation of Enroll Kzoo County. We knew we
couldn’t do it alone so we engaged partners in order to help achieve this goal. We thought it is
important to educate the people about the need for health insurance and most people know that
but connecting them to actually going through the process of getting it is another matter, so that
is what we really focused on, providing that technical assistance to get community members
enrolled.
Â
S: Had Bronson participated in this type of collaborative process before?
F: Yes, a variety of things, things like Healthy Babies, Healthy Starts, over the years there has
a been a number of collaborative efforts that we have been involved with; which reflects the fact
that “we recognize the hospital is one piece of a very complex puzzle and so we need to engage
other community partners, in fact that effort has even intensified within the hospital, we our held
accountable not just for the patients stay while there in the in the hospital but also increasingly
once they go home 30, 60, and 90 days out ,we are measured by that…
It has always been important, but now it’s absolutely critical that we create connections within the community.
S: How do you think the ACA will affect Kzoo?
F: I think it is very important, for years and I know there has been a great debate on this issue.
It has become very political and polarizing, my feeling is that the health care industry has been
advocating for years that one of the flaws historical is, you have the insuranced population and
the uninsured population, and although the uninsured has access to health care, its usually
not at the right time or place. Meaning that if people don’t have insurance they seek health
care in the E.R, and they are seeking primary care in the ER, and of course we are equipped
to provide that but the ER dept. is probably the most expensive place for health care to be
delivered and there are better ways to deliver primary and secondary care other than in the ER,
as a result there has been a hidden tax on those who have insurance rather it is an individual
or an employer that provides insurance, because those insurance rates have to somehow
compensate for those that don’t have insurance, so there has been this hidden tax that has
been referred to, and so “the health care industry has advocated for years that if everyone
had coverage it would be a more equitable system and I think philosophically we embrace the
concept that people have a right to health are coverage, but unfortunately it has become very
politicized, and my feelings is the ACA isn’t perfect however, I think it takes a big step with the
requirement that everyone have health insurance, because you really need this large pool of
everyone being covered for the system to work, so I am generally supportive, I don’t think the
law is perfect, but I would rather work on improving it with this starting point because I think
it has taken this country years, decades getting to this point of finally figuring out a way, other
people have different opinions, but we finally have gotten something done, now we need to just
improve it.
 S: Your thoughts on the possible shortage of primary care givers?
F: Yes, for economically reasons more people have been choosing to go into specialized
fields instead of primary care so there is a trend right now of having a shortage of primary care
doctors, one way we are addressing this is by looking at the whole way primary care is being
delivered, we are emphasizing a team approach, where a physician would be managing and
supervising the care but the care could be delivered by a nurse practitioner or a physician
assistants, as well as other members of the team, a lot of the time that physicians spend with
the patient, maybe could be better delivered by a social worker or a psychologists, we are
working on developing a model where the patients total needs can be addressed, but the
physician can be part of the team as opposed to the only one seeing that patient, which can
result in better care for the patient.
 S: How will this affect the E.R?
F: We continue to see an increasing amount of patients in the ER, with more people with
insurance we expect that to even increase more. Â The trick is coming up with the right mix of
care providers, and that’s why the number one priority under this community healthy catalyst
goal is improving access, we use this mantra the right care, right time, right place, right cost,
so we are looking at all the entry points for patients coming into the system, and trying to tailor
those access points to the patient needs.
S: Other thoughts on improving access?:
F: We have just recently added what we call fast care, a retail setting in Meijer on Westnedge,
that provides another option for people who just need like kids needing a sports physical or
children needing immunizations, simple things that can be delivered by a nurse practitioner,
we have also extended hours in some of our practices, by including now evening and weekend
hours, we have also opened a new practice that is piloting this concept where there is a whole
team approach to care, we are looking at a variety options and we call all of these initiatives
together, Primary Care 2.0, the advance version of primary care. The other important aspect to
improving access it the Family Health Center, with the recent grant they received they will be
able to provide more access to community members.
S: Do you think education is key to helping people get access?
F: Absolutely, I personally have referred some people to the events, and it’s so interesting
to hear the misconceptions, and many people assume they can’t afford it. I just read in the
Economist, of the people enrolled so far, over a quarter did not have health insurance before, I
thought that was a good objective assessment, because again this issue has been so politicized
and you get information and misinformation, so it was great to see a respected publication
like the Economist do an analysis. I think we need to give it time; see how it evolves, one of
the initial criticisms was how many of the 8 million, who have enrolled, are going to pay their
premiums and there has already been a study done and the insurance companies themselves
have indicated that there has been a pretty high percentage of people who not only enrolled but
also are paying their premiums, so that debunks yet another myth about it, the remaining issue
is whether there will be the appropriate distribution of age ranges, because if it tends to skew
towards an older population, you are not going to get the appropriate proportion of people, that
are not heavy utilizers of care, I think it is still early to know the final numbers on what that is.
S: What do you think some of the biggest barriers were in getting people enroll?
F: Well, certainly the launch was less than perfect; it did slow down the initial enrollment and
it just fueled the negative arguments about it, so that was one factor. Â The second factor is the
lack of understanding, not understanding what your options are, there is a learning curve, some
people have never had health insurance so it can be confusing. I think education is the key to it
and I think having good objective information about what is working and what’s not working and
if it’s not working what do we need to address those issues.
S: In the end, what is one thing you wish people knew?
F: To do your homework and really get to understand the facts and not be swayed into the
polarized opinions either way, because I don’t think it is going to solve all of our problems on
one hand, but on the other I think there is a lot of good that can come out of it, so I think be
objective, be patient and really get the facts before making a decision. I have heard a lot about
how we need to get rid of this act but keep some of the provisions, such as children up to 26
being able to be covered, people like that part, the objective answer to that though is; is you
cant have all the provisions that people like, without provisions such as individual mandate
because you have to have that broad population enrolled in order for the whole plan to work
economically. In the end, be objective and know the facts.
Image from mlive.com