By Madeline LeVasseur
Postnatal care involves an immensely critical time in the life of a newborn and its mother. Over two-thirds of all newborn deaths occur in their first week of life, and half of these deaths occur in the first twenty-four hours. In Kalamazoo, the disparity in infant mortality between black and white babies makes this first period of life even more crucial to addressing the rate of black infant mortality in our community. In focus groups with community members, Black mothers have expressed shared feelings of being rushed through this vital period of care after giving birth. Healthcare workers expressed speculations about the degree of respect that mothers are receiving in Kalamazoo and discussed the negative impact of not having a racially diverse staff to interact with a racially diverse community. To address the problem of black infant mortality in the context of postnatal care, we recommend increasing the amount of care after delivery with increased home visits to mothers and their newborns. Furthermore, it is recommended that health facilities require racism training for all staff in order that the relationship between mothers and healthcare professionals be significantly improved.
The death of any infant is a tragedy. This seems to be the point that no one in the Kalamazoo community, resident or health professional, is debating. Infant death is a tragedy. Where the discussion of infant mortality in Kalamazoo continues then, is what several health professionals refer to as a “puzzle” of a problem: the complex web of interrelated factors—social, medical, and environmental—that result in infant mortality. The even more concerning piece of this puzzle is the disparity of infant mortality between blacks and whites in Kalamazoo. A disparity that has greatly increased since 2001 as the overall rate of infant mortality in Kalamazoo has been declining (Michigan Department of Community Health, Division for Vital Records and Health Data Development. Michigan Infant Death Statistics. March, 2014.) This is the difficult situation that is Kalamazoo today. This is the complex framework in which our discussion of infant mortality ought to take place. It should be acknowledged that postnatal care, while incredibly important to the survival of our infants, is one of many compounding elements in the discussion of infant mortality in Kalamazoo.
Postnatal care involves a very critical time in the life of a newborn child; receiving proper postnatal care can genuinely be a matter of life or death for that infant. The World Health Organization reports that of the 2.9 million newborns who died in 2012, nearly half of them died within their first 24 hours of life (World Health Organization, Postnatal Care, 2015). Including this crucial first day of life, more than two-thirds of newborn deaths will occur by the end of their first week after delivery (Stines et. al, 2007). Nuru-Jeter et. al write that “low birthweight (< 2,500 g) and preterm delivery (<37 weeks) are two to three times more likely among African-Americans than Non-Hispanic Whites” (Nuru-Jeter et. al, 2008). Such a disparity illustrates that this critical time is even more relevant to the discussion of black infant mortality. Regardless of the factors that lead to the preterm birth of an infant or resulted in an infant with low birthweight, the availability of postnatal care in the immediate time following the birth will determine the outcome of the situation.
The need in Kalamazoo for postnatal care in the immediate period after birth is very evident. According to one Kalamazoo social worker, the Neonatal Intensive Care Unit (NICU) of Bronson Hospital admits around 600 infants a year, and experiences approximately 10 to 12 deaths a year in those newborns that are admitted to the nursery (Focus Group: Bronson Social Workers, 2015). The infants passing through the NICU of Bronson Hospital represent the cases of extreme health conditions; however, all infants need to receive some level of postnatal care following their birth. According to the World Health Organization, this basic level of care should include promoting early and exclusive breastfeeding, keeping the baby warm, increasing hand washing and providing hygienic umbilical cord and skin care. Furthermore, such care should include identifying conditions that require additional care of the infant or admission to a health facility (World Health Organization, Postnatal Care, 2015).
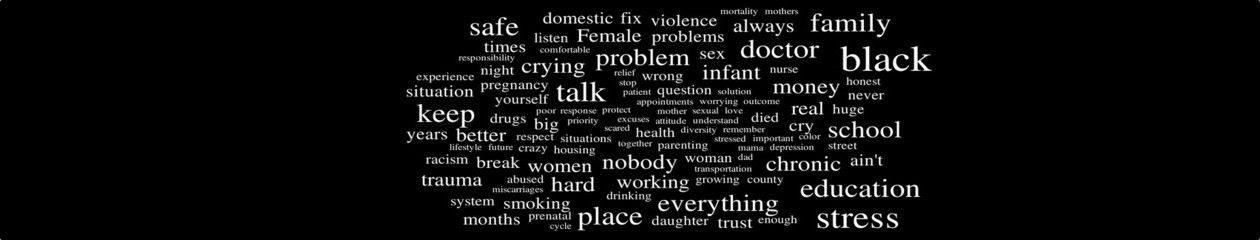
In Kalamazoo, it seems that postnatal care is one of the areas where the disparity between black and white becomes very evident. While many health professionals in focus groups reported that they felt they were providing equal levels of treatment, care, and resources, black mothers in the Kalamazoo community spoke from a different perspective. When speaking about why the hospital would send a baby home before it should, one mother said, “That’s because we’re African Americans. I’m sorry to say, it’s African Americans that they let go because we only receiving Medicaid” (Focus Group: YWCA, 2015). The resources and the care that the health professionals see in Kalamazoo are not what the community members are seeing. A second mother spoke with the same opinion.
[Hospital workers] throw you out in the street. Throw you babies out in the street like, ‘who gives a damn about you. Another black person, black baby gone—Bye-bye. So we ain’t got to worry about that baby growing up, carrying no gun, or being a hoe on the corner.’ That’s just how I look at it. That’s my point. Because if it was a Caucasian baby, a middle-class baby, they would have been up in there. That baby would have been taken care of (Focus Group: YWCA, 2015).
The problem in Kalamazoo, it would appear, is a communication problem. A disconnect. Opinions expressed throughout various focus groups illustrated a feeling of isolation and a lack of communication not only between resources in the community, but as shown by the quotes above, between the health professionals and the community they are servicing.
This is not to say, however, that medical professional and healthcare workers are not aware of this disconnect. One nurse at Bronson Hospital shared her speculations about the level of respect that patients were receiving. “So if patients are getting that level of special treatment and respect and compassion, where they feel like they are being listened to and they want to come back. And it’s not just put this on your tongue, step on that scale, everything looks fine, see you next time” (Focus group: Bronson labor and delivery nurses, 2015). The importance of this component in postnatal care is significant. If mothers do not feel like they are being respected by the health professionals overseeing their treatment, as was expressed by the community members quoted earlier, why would they be expected to continue seeking treatment and care from these facilities? When the life of infants and the health of mothers is what is at risk, health professionals should be doing all that is possible to create positive experiences with these patients and providing respectful treatment that will allow for continued professional relationships between workers and mothers.
While respectful treatment was one factor considered in focus groups with the Kalamazoo community, the racial diversity of staff at health facilities was another recurring topic. Nurses, social workers, and other healthcare personnel all discussed the impact that having a diverse staff could have on interactions with mothers and families in Kalamazoo. “In our community if you take a look at the other programs they don’t really culturally represent the community that they’re trying to serve. Their heart is probably there, but it’s not the diversity that is needed in the home visitation group to represent high-risk groups” (Focus group: healthy babies, healthy start, 2015). Many of the healthcare workers participating in focus group interviews had speculations echoing this opinion. Workers appear to be skeptical of the impact white medical personnel can have telling a black mother what she has to do. Their doubts are based in research and studies that have shown the impact such a racial difference can have on worker-patient interactions. “It’s been proven that people feel more comfortable when the people who come in can at least relate to them in some way, culturally, or whatever it may be” (Focus group: healthy babies, healthy start, 2015).
Taking all of this into consideration then, what is Kalamazoo supposed to do? Where does the community go from here to address the issue of black infant mortality? For a problem with numerous contributing factors, the answer cannot be singular. In regards to postnatal care, it seems there are several recommendations to be made. The first comes from a set of guidelines provided by the World Health Organization in 2013. Due to the critical nature of the postnatal period, the WHO recommends increased contact with the mother and infant after release from the health facility. It is recommended that after the first 24 hour period, three additional visits should be made: one on the third day after birth, one between 7-14 days after birth, and another six weeks after the birth (WHO, WHO recommendations on postnatal care of the mother and newborn, 2015). Increased interactions between the healthcare personnel and mothers in Kalamazoo will help to address the postnatal period and provide the necessary care that these black mothers felt they had not received.
A second recommendation comes from the discussions that Kalamazoo health professionals had about patient respect and staff diversity. To restructure a health facility’s procedures or staff is a difficult task and perhaps an unrealistic suggestion. Ideally, health workers would be representative of the community they provide for. However, when the circumstances do not result in this, it seems that continued staff training is both necessary and important. It has been identified and acknowledged that the relationship between healthcare workers and mothers in Kalamazoo is not to the standard it needs to be. Black mothers in Kalamazoo expressed that they felt they were not cared about, and healthcare workers expressed concerns that they were unable to connect with certain target groups in the community. To address the disconnect between workers and these patients, the first step should be required racism training for all employees. Establishing the importance of cultural competency, particularly in the context of black infant mortality, will significantly improve these worker-patient relationships. This will not only improve the level of care being received during the postnatal period (especially during home visits), but also during all other times of interaction with patients. In a diverse community such as Kalamazoo, it seems that the value of requiring such staff training in both evident and substantial.